Polycystic Ovarian Syndrome (PCOS) is a common hormonal disorder affecting an estimated 6% to 13% of women of reproductive age globally. Medical experts increasingly recognize PCOS not just as a fertility issue, but as a complex, lifelong multisystem disorder with significant implications for metabolic and cardiovascular health.
Understanding the Hormonal Imbalance
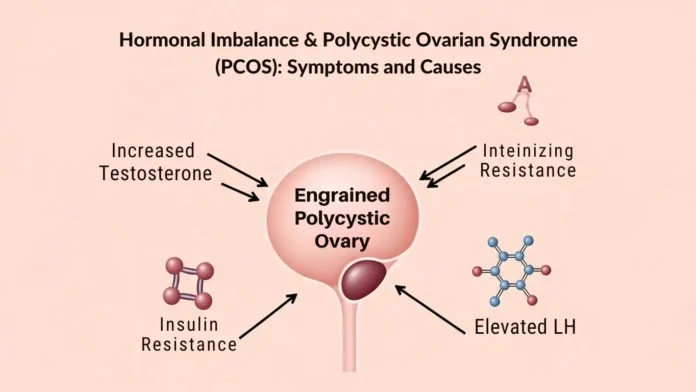
At its core, PCOS is driven by an imbalance of reproductive hormones. In a typical cycle, the ovaries produce small amounts of androgens (often called “male hormones”). In individuals with PCOS, the ovaries produce abnormally high levels of these hormones, particularly testosterone.
This excess of androgens can disrupt the development and release of eggs during ovulation. Instead of being released, the eggs may remain in the ovaries as small, fluid-filled sacs or follicles, which can appear as “cysts” on an ultrasound.
Common Symptoms of PCOS
Symptoms often begin around the time of the first menstrual period but can develop later in response to significant weight gain or lifestyle changes.
- Irregular Periods: This is the most common sign. It includes missing periods, having fewer than nine periods a year, or having cycles longer than 35 days.
- Hirsutism: Excess dark, thick hair growth on the face, chin, chest, belly, or back, affecting up to 70% of those with the condition.
- Severe Acne: Persistent acne on the face, chest, and upper back that may continue well past teenage years.
- Weight Gain: Difficulty maintaining a healthy weight, with weight often concentrating around the abdomen (sometimes called “PCOS belly”).
- Thinning Hair: Male-pattern baldness or thinning hair on the scalp.
- Skin Changes: Darkening of skin (acanthosis nigricans) in folds like the neck, groin, and armpits, or the appearance of skin tags.
- Infertility: PCOS is a leading cause of female infertility due to irregular or absent ovulation.
Primary Causes and Risk Factors
While the exact cause of PCOS remains unknown, research in 2026 points to a combination of genetic and environmental factors.
- Insulin Resistance: Up to 80% of women with PCOS have insulin resistance. When the body cannot use insulin effectively, the pancreas produces more, which in turn triggers the ovaries to produce excess androgens, further disrupting ovulation.
- Genetics: PCOS often runs in families. If a biological parent or sister has the condition, your risk is significantly higher.
- Low-Grade Inflammation: People with PCOS often have chronic, low-grade inflammation that stimulates polycystic ovaries to produce more androgens.
- Environmental Factors: Emerging 2025 research suggests exposure to certain endocrine-disrupting chemicals (EDCs) and pollutants may contribute to the development of the syndrome.
Long-Term Health Risks
Untreated PCOS is now classified as a cardiovascular risk-enhancing condition. Long-term complications can include:
- Type 2 Diabetes: More than half of women with PCOS develop type 2 diabetes by age 40.
- Heart Disease: Increased risk of high blood pressure, high cholesterol, and stroke.
- Endometrial Cancer: Infrequent periods lead to a thickened uterine lining, which increases the risk of cancer in the lining of the uterus.
- Mental Health Issues: Depression and anxiety are 3 to 8 times more common in those with PCOS.
- Sleep Apnea: Particularly common in those who are overweight.
Diagnosis and Next Steps
Standard diagnosis (using the Rotterdam Criteria) typically requires meeting at least two of the following:
- Irregular or absent periods.
- Signs or blood tests showing high androgen levels.
- Polycystic ovaries visible on an ultrasound.
If you are experiencing these symptoms, consult a healthcare provider for a comprehensive evaluation. Early management through lifestyle changes and medication can significantly reduce long-term health risks.
Final Thought
Polycystic Ovarian Syndrome (PCOS) is more than a reproductive condition it is a lifelong hormonal and metabolic disorder that requires awareness, early diagnosis, and ongoing management. With the right medical guidance, lifestyle changes, and support, individuals with PCOS can effectively manage symptoms, reduce long-term health risks, and lead healthy, fulfilling lives. Empowerment begins with understanding, and seeking timely care is a crucial step toward better overall well-being.